This report provides an update through June 2023 of routine screening results for antibodies to the human immunodeficiency virus among members of the U.S. military. Consistent with prior year reports, the HIV-antibody seropositivity rate for 2022 among Army active component service members (0.25 per 1,000 soldiers tested) remained above active component members of the Air Force (0.17 per 1,000 airmen tested), Navy (0.16 per 1,000 sailors tested), Coast Guard (0 per 1,000 Coast Guardsmen tested), and Marine Corps (0.11 per 1,000 Marines tested). In comparison to 2022, the mid-year HIV seropositivity rates as of June 2023 declined for active component service members of the Army and Air Force but increased for the Navy and Marine Corps.
What are the new findings?
From January 2018 through June 2023, approximately 7 million U.S. military service members (active component, reserve component, and national guard) were tested for antibodies to HIV, and 1,502 were identified as HIV-antibody positive (seropositivity: 0.21 per 1,000 tested). The rate among men persisted above women throughout the surveillance period.
What is the impact on readiness and force health protection?
For over 30 years, the routine screening for antibodies to HIV has enabled the U.S. military to provide adequate and timely medical care to infected service members. Future studies should fully describe seropositivity rates by age and race, to further elucidate trends for the most at-risk populations. Additionally, health-seeking behaviors and co-morbidities should be evaluated to identify those at highest risk for HIV infection.
Background
The Department of Defense has conducted an active surveillance program for HIV since 1986, when reliable screening methods for the virus became widely available. The DOD surveillance program consists of screening all service members at specific points in time: prior to entry (all accessions must be HIV-negative prior to start of service), before deployment or any change in status (change in component, between branches, or commissioning), and once every 2 years while a military member.1
Before 2009, the DOD screening program employed laboratory techniques that detected only HIV-1-type infections. Since 2009, all programs have adopted methods that detect antibodies to HIV-1 and HIV-2. Although HIV-2 infection is rare in the U.S., it is more prevalent in other parts of the world where service members may support military operations. This report refers to the target of the screening programs as simply “HIV” without specifying types.
Infection with HIV is medically disqualifying for entry into service with the U.S. military. Following significant advances in the diagnosis, treatment, and prevention of HIV, in June 2022 the DOD updated its policy, preventing the discharge or separation of service members living with HIV who have an undetectable viral load solely on the basis of their HIV-positive status.1 In addition, HIV-positive personnel are not non-deployable solely for a positive status; decisions on deployability are made on an individual basis and must be justified by the service member’s inability to perform the duties to which he or she would be assigned.2
Summaries of HIV seropositivity for members of the U.S. military have been archived with the MSMR since 1990. This report summarizes numbers and trends of newly identified HIV-antibody seropositivity from January 1, 2018 through June 30, 2023 among military members of the active and reserve components of 5 services under the U.S. Armed Forces, as well as the Army National Guard and Air Force National Guard.
Methods
The surveillance population included all individuals eligible for HIV antibody screening from January 1, 2018 through June 30, 2023 while serving in the active or reserve component of the Army, Navy, Air Force, Marine Corps, or Coast Guard. All individuals who were tested and all first-time detections of antibodies to HIV through U.S. military medical testing programs were ascertained from the Department of Defense Serum Repository specimens accessioned to the Defense Medical Surveillance System. Due to data availability issues, the Navy and Marine Corps new HIV seropositive numbers for 2023 were obtained by the Navy Bloodborne Infection Management Center from the Navy’s HIV Management System.
An incident case of HIV-antibody seropositivity was defined as an individual with positive HIV test results from 2 serial specimens. Individuals who had just 1 positive result without a subsequent negative result were also defined as positive, to capture those who had yet to test positive a second time.
Annual rates of HIV seropositivity among service members were calculated by dividing the number of incident cases of HIV-antibody seropositivity during each calendar year by the number of individuals tested at least once during the relevant calendar year. Rates were further stratified by service, component, and sex. Overall rates by age category were calculated for all services for the full annual years of 2018 through 2022.
Results
Overall
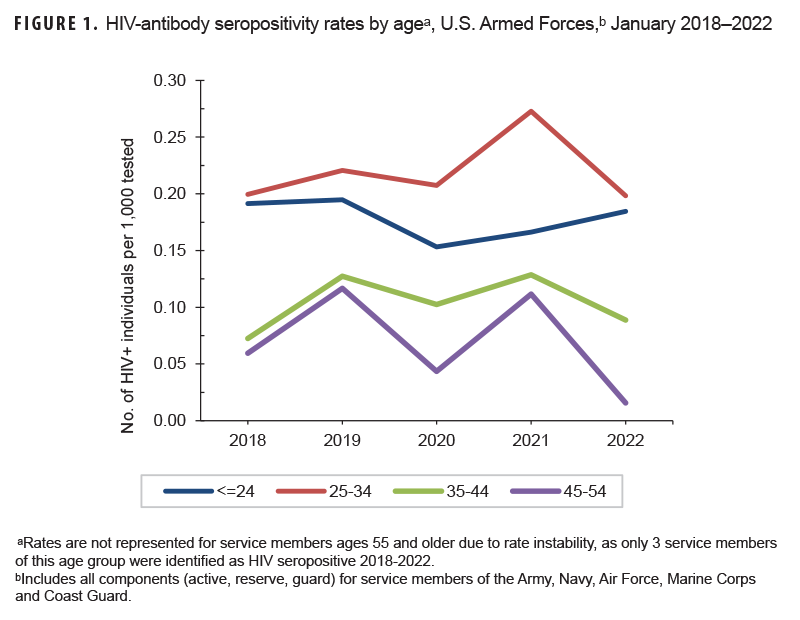
From January 2018 through June 2023, approximately 7 million service members (active component, Guard, and reserve) were tested for antibodies to HIV, and 1,502 were identified as HIV-antibody positive (seropositivity: 0.21 per 1,000 tested) (data not shown). The rate among males (0.25 per 1,000 tested) persisted above females (0.03 per 1,000 tested) throughout the surveillance period, as only 39 females were identified as newly HIV antibody-positive during this time. Age-specific HIV seropositivity rates are presented for complete annual years in Figure 1; service members 25 to 34 years of age represented the highest age-specific rates from 2018 to 2022.
U.S. Army
Active component
From January 2022 through June 2023, a total of 444,341 soldiers in the active component of the U.S. Army were tested for antibodies to HIV, and 106 soldiers were identified as HIV-antibody positive (seropositivity: 0.24 per 1,000 soldiers tested) (Table 1).
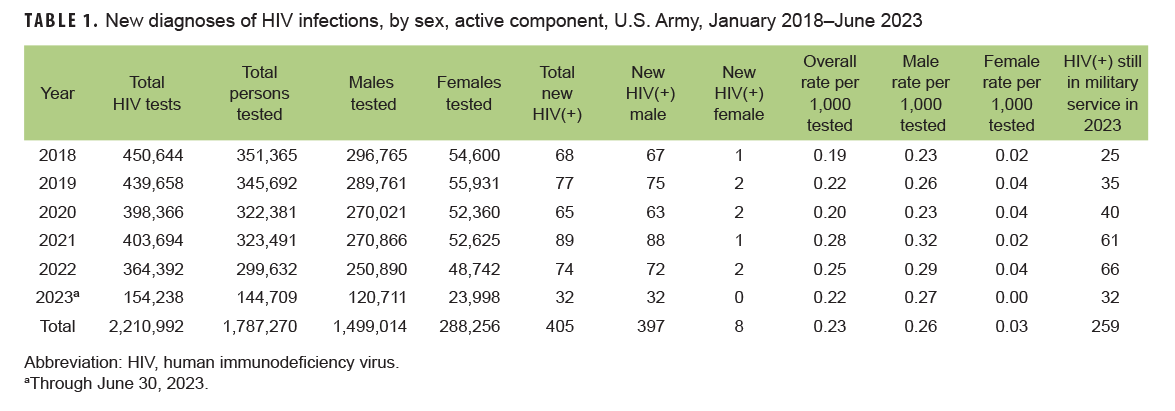
During the surveillance period, annual seropositivity rates fluctuated between a low of 0.19 per 1,000 tested in 2018 and a high of 0.28 per 1,000 tested in 2021 (Table 1, Figure 2). Annual seropositivity rates for male active component soldiers were considerably higher than those of female active component soldiers (Figure 2).
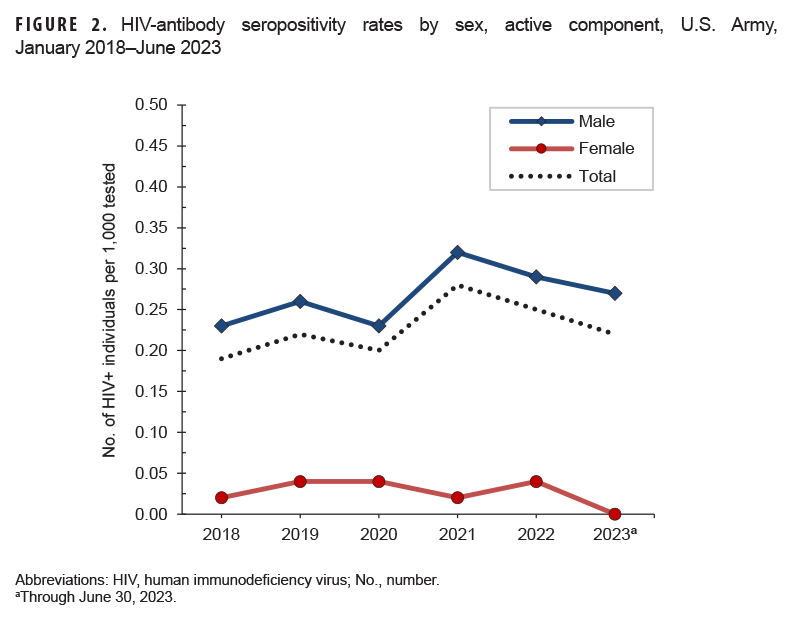
During 2022, on average, 1 new HIV infection was detected among active component soldiers per 4,924 screening tests (Table 1). Of the 405 active component soldiers diagnosed with HIV infections since 2018, a total of 259 (63.9%) were still in military service in 2023.
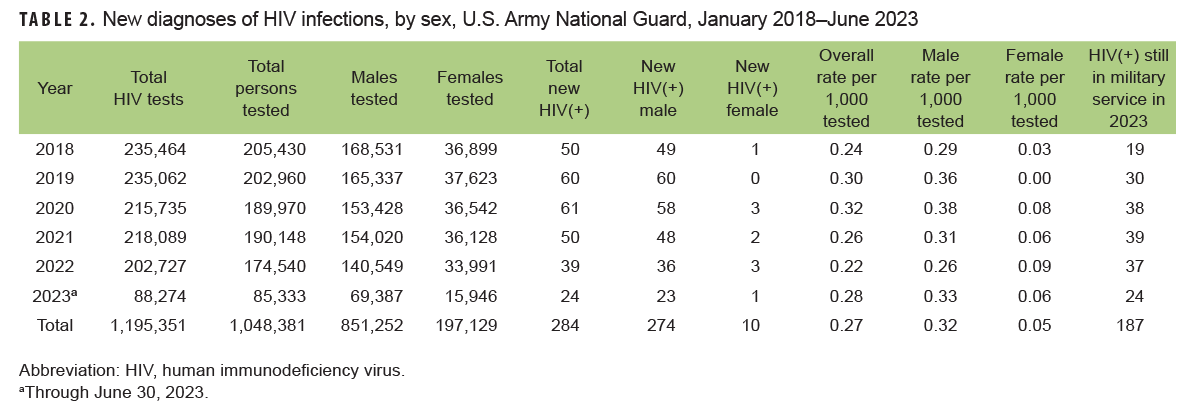
Army National Guard
From January 2022 through June 2023, a total of 259,873 members of the U.S. Army National Guard were tested for antibodies to HIV, and 63 soldiers were identified as HIV-antibody positive (seropositivity: 0.24 per 1,000 soldiers tested) (Table 2). On average, during 2022, 1 new HIV infection was detected among Army National Guard soldiers per 5,189 screening tests. Of the 284 National Guard soldiers who tested positive for HIV since 2018, a total of 187 (65.8%) were still in military service in 2023.
Army Reserve
From January 2022 through June 2023, a total of 119,195 members of the U.S. Army Reserve were tested for antibodies to HIV, and 46 soldiers were identified as HIV-antibody positive (seropositivity: 0.39 per 1,000 soldiers tested) (Table 3). During 2022, on average, 1 new HIV infection was detected among Army reservists per 3,025 screening tests. Of the 180 Army reservists diagnosed with HIV infections since 2018, a total of 114 (63.3%) were still in military service in 2023.

U.S. Navy
Active component
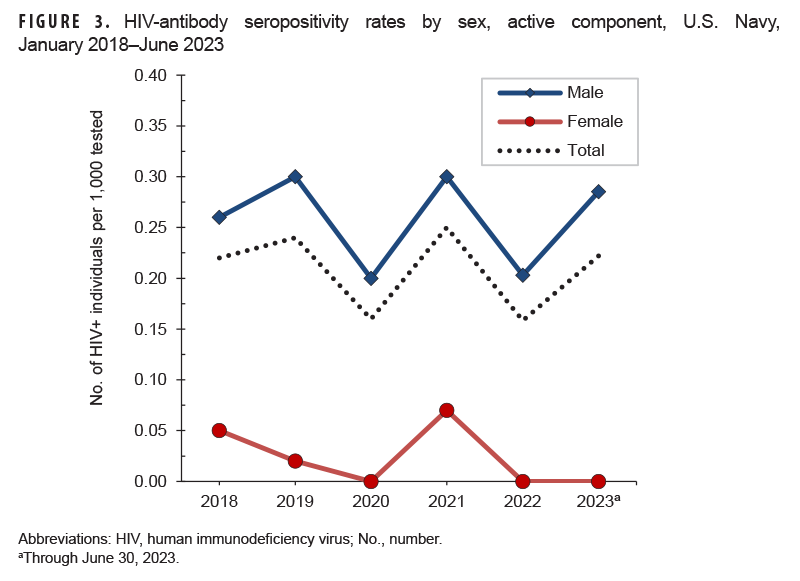
From January 2022 through June 2023, a total of 294,801 active component members of the U.S. Navy were tested for antibodies to HIV, and 53 sailors were identified as HIV-antibody positive (seropositivity: 0.18 per 1,000 sailors tested) (Table 4).
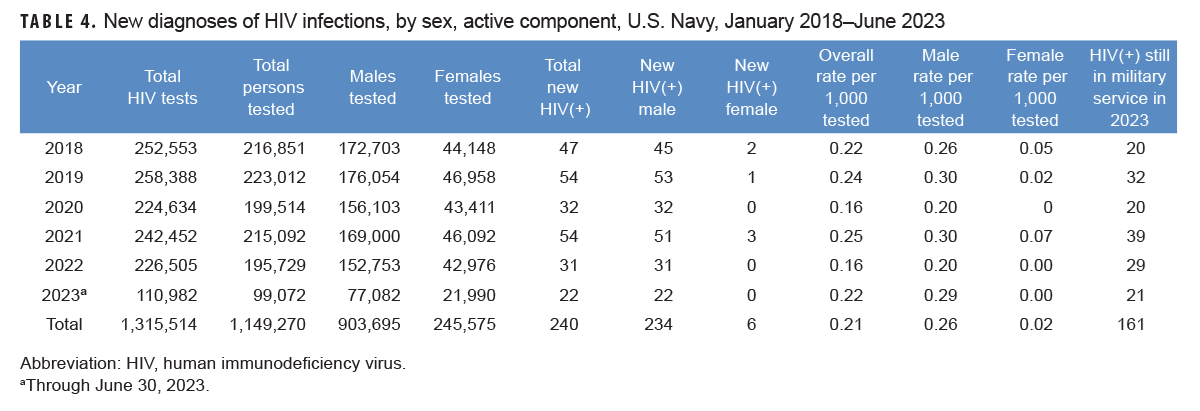
During 2022, on average, 1 new HIV infection was detected among active component sailors per 7,306.6 screening tests. Of the 240 active component sailors who tested positive for HIV since 2018, a total of 161 (67.1%) were still in military service in 2023. During each year of the surveillance period, only 0 to 3 female sailors tested positive. Among male sailors, the rate per 1,000 tested fluctuated between 0.20 to 0.30 from 2018 through 2022 (Figure 3).
Navy Reserve
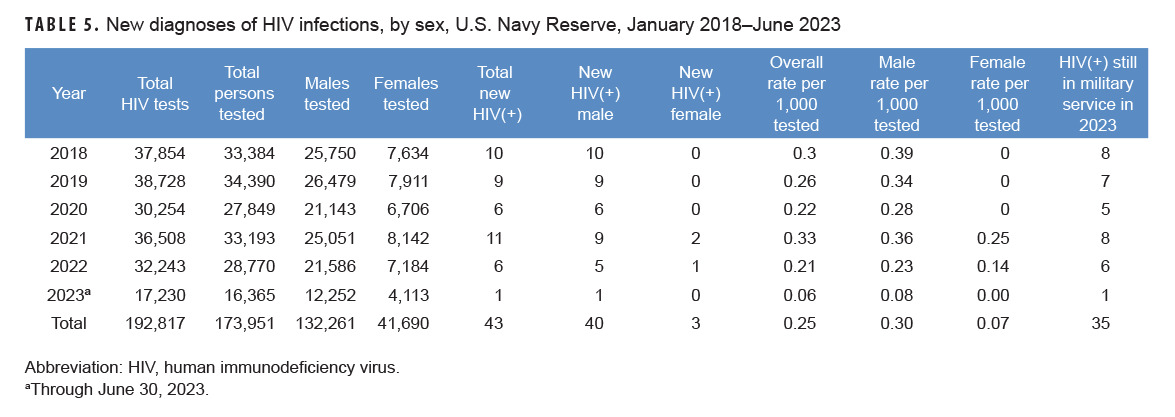
From January 2022 through June 2023, a total of 45,135 members of the U.S. Navy Reserve were tested for antibodies to HIV, and 7 sailors were identified as HIV-antibody positive (seropositivity: 0.16 per 1,000 sailors tested) (Table 5). On average, during 2022, 1 new HIV infection was detected among Navy reservists per 5,373.8 screening tests. Of the 43 reserve component sailors diagnosed with HIV infections since 2018, a total of 35 (81.4%) were still in military service in 2023. The HIV-antibody seropositivity rate declined from 0.21 per 1,000 Navy reservists in 2022 to 0.06 as of June 2023.
U.S. Air Force
Active component
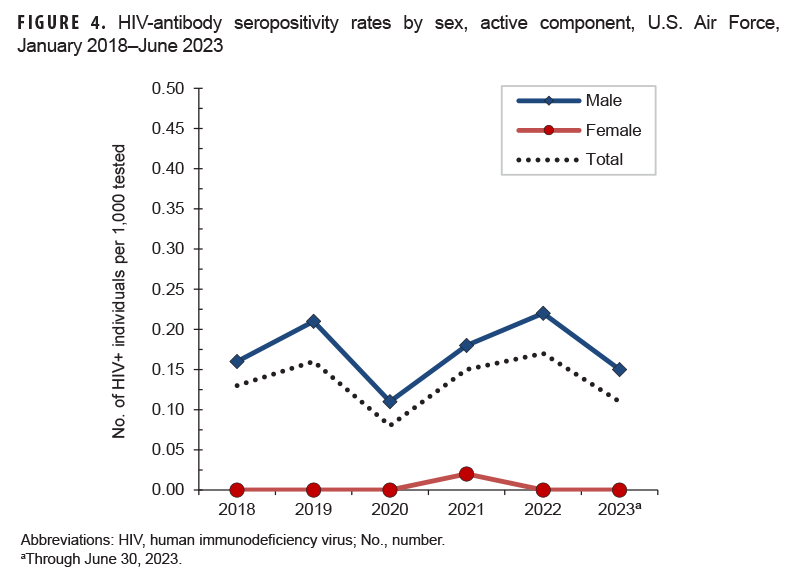
From January 2022 through June 2023, a total of 286,900 active component members of the U.S. Air Force were tested for antibodies to HIV, and 43 Air Force members were diagnosed with HIV infection (seropositivity: 0.15 per 1,000 Air Force members tested) (Table 6).
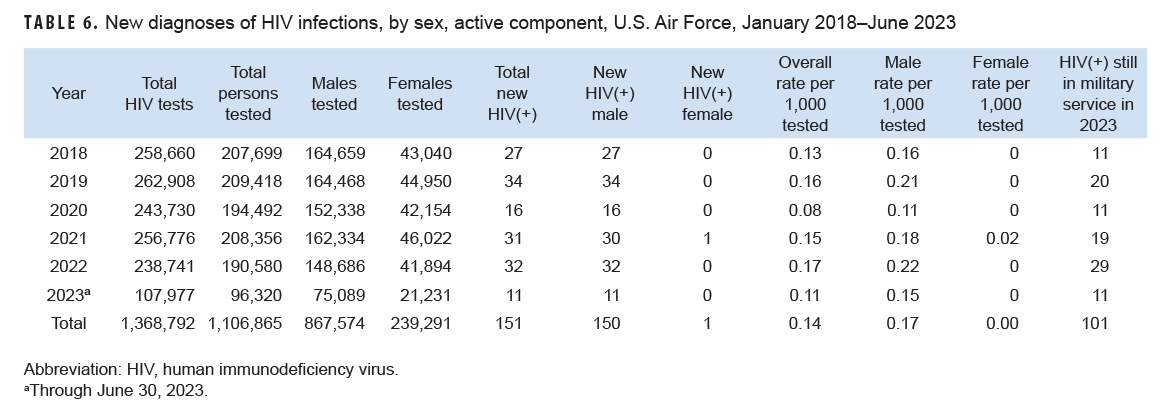
On average, 1 new HIV infection was detected among active component Air Force members per 7,461 screening tests in 2022. Of the 151 active component Air Force members diagnosed with HIV infections since 2018, 101 (66.9%) were still in military service in 2023. During the surveillance period, seropositivity rates among male members ranged from a low of 0.11 per 1,000 tested in 2020 to a high of 0.22 per 1,000 tested in 2022 (Figure 4).
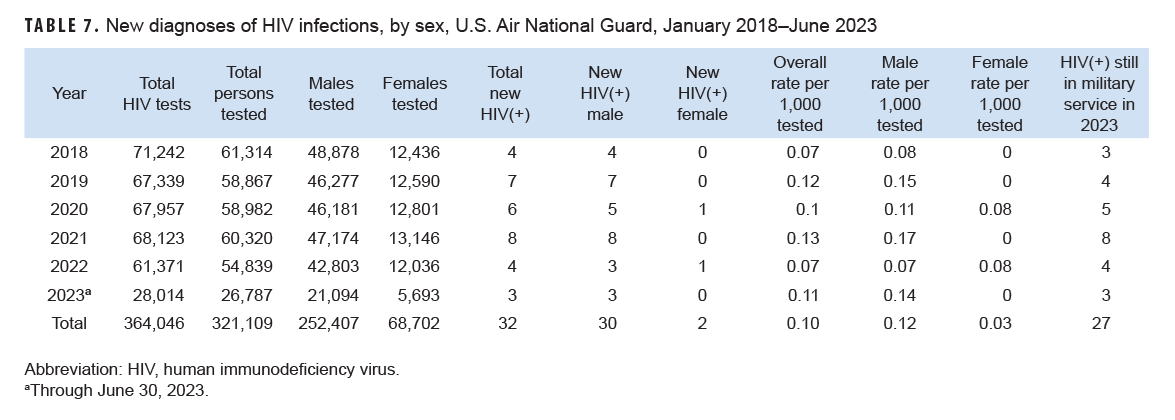
Air National Guard
From January 2022 through June 2023, a total of 81,626 members of the Air National Guard were tested for antibodies to HIV, and 7 Air National Guard members were diagnosed with HIV infection (seropositivity: 0.09 per 1,000 airmen tested) (Table 7). During 2022, on average, 1 new HIV infection was detected among Air National Guard members per 15,343 screening tests. Of the 32 Air National Guard members diagnosed with HIV infections since 2018, 27 (84.4%) were still in military service in 2023.
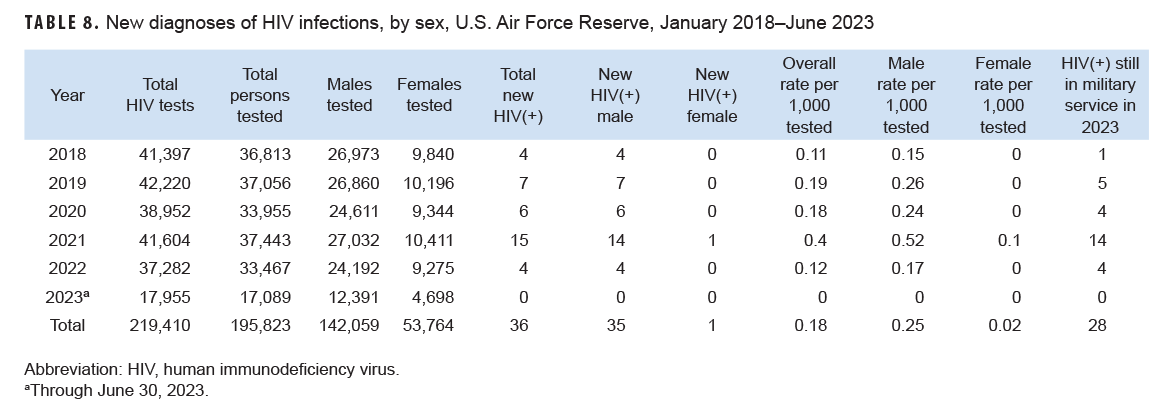
Air Force Reserve
From January 2022 through June 2023, a total of 50,556 members of the Air Force Reserve were tested for antibodies to HIV, and 4 Air Force reservists were diagnosed with HIV infections (seropositivity: 0.08 per 1,000 airmen tested) (Table 8). During 2022, on average, 1 new HIV infection was detected among Air Force reservists per 9,321 screening tests. Of the 36 Air Force reservists diagnosed with HIV infections since 2018, 28 (77.8%) were still in military service in 2023.
U.S. Marine Corps
Active component
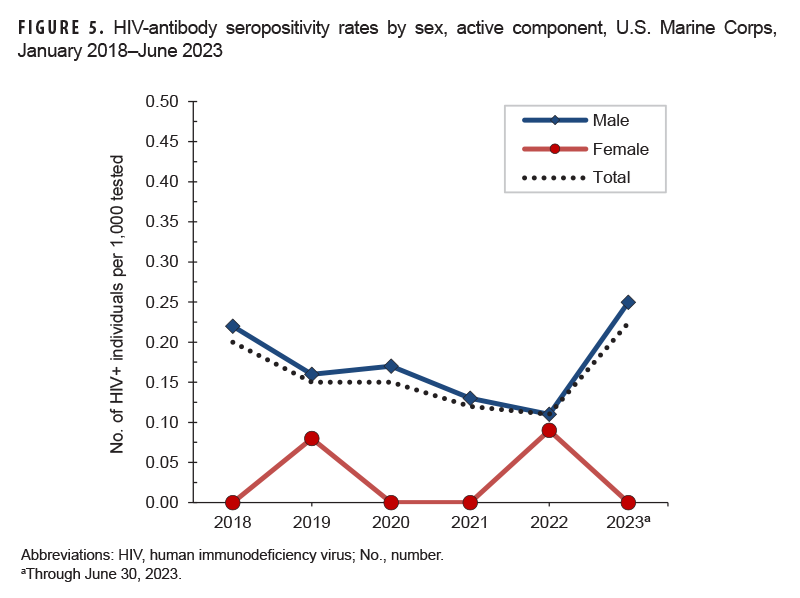
From January 2022 through June 2023, a total of 166,411 members of the active component of the U.S. Marine Corps were tested for antibodies to HIV, and 24 Marines were identified as HIV-antibody positive (seropositivity: 0.14 per 1,000 Marines tested) (Table 9).

During 2022, on average, 1 new HIV infection was detected among active component Marines per 10,790 screening tests. Of the 106 active component marines diagnosed with HIV infections since 2018, a total of 47 (44.3%) were still in military service in 2023. Among males, the rate per 1,000 declined from 0.22 per 1,000 tested in 2018 to 0.11 per 1,000 tested in 2022, thereafter increasing to a rate of 0.25 per 1,000 tested as of June 2023 (Figure 5).
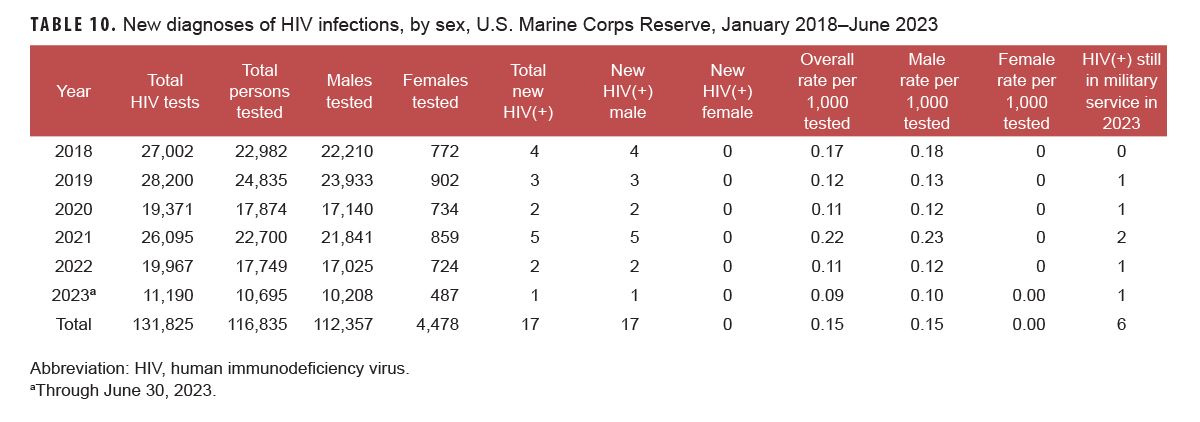
Marine Corps Reserve
From January 2022 through June 2023, a total of 28,444 members of the U.S. Marine Corps Reserve were tested for antibodies to HIV, and 3 Marine Corps reservists were identified as HIV-antibody positive (seropositivity: 0.11 per 1,000 Marines tested) (Table 10). During 2022, on average, 1 new HIV infection was detected among Marine Corps reservists per 9,983.5 screening tests. Of the 17 Marine Corps reservists diagnosed with HIV infection since 2018, a total of 6 (35.3%) were still in military service in 2023.
U.S. Coast Guard
Active component
From January 2022 through June 2023, a total of 27,896 members of the active component of the U.S. Coast Guard were tested for antibodies to HIV; 0 were identified as HIV-antibody positive (Table 11).
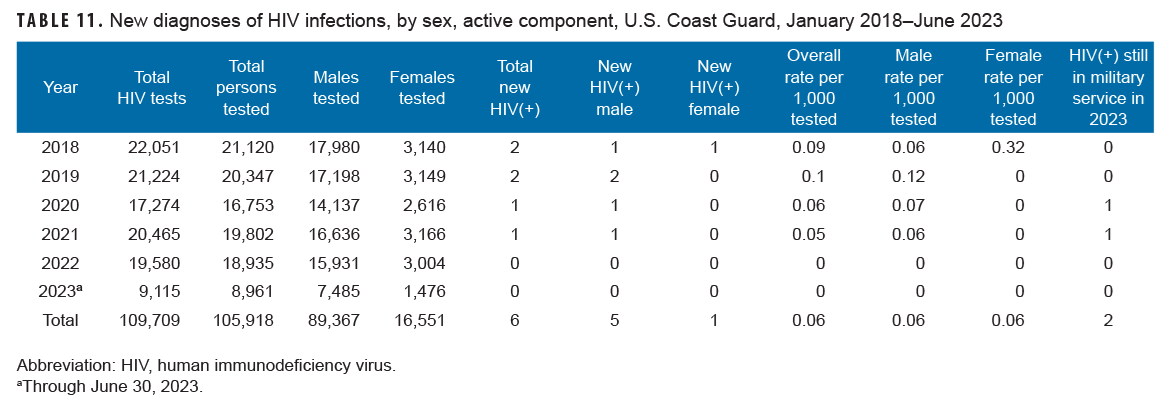
Of the 6 active component Coast Guardsmen diagnosed with HIV infections since 2018, a total of 2 (33.3%) were still in military service in 2023.
Coast Guard Reserve
From January 2022 through June 2023, a total of 4,354 members of the U.S. Coast Guard Reserve were tested for antibodies to HIV; 0 Coast Guard reservists were identified as HIV-antibody positive (Table 12).

Discussion
The U.S. military has conducted routine screening for antibodies to HIV among all civilian applicants for service and all service members for more than 30 years.3-6 Results of U.S. military HIV-antibody testing programs have been summarized in the MSMR for more than 2 decades.7 This year marks the returned inclusion of HIV screening for active and reserve component service members of the U.S. Coast Guard, to include summary data for 5 services of the U.S. Armed Forces.
This report documents that the full-year HIV-antibody seropositivity rate in 2022 among Army active component service members (0.25 per 1,000 soldiers tested) remained greater than among active component members of the Air Force (0.17 per 1,000 airmen tested), Navy (0.16 per 1,000 sailors tested), Coast Guard (0 per 1,000 Coast Guardsmen tested), and Marine Corps (0.11 per 1,000 Marines tested). In comparison to 2022, the mid-year HIV seropositivity rates as of June 2023 declined for active component service members of the Army and Air Force but increased for the Navy and Marine Corps.
The 2022-2025 National HIV/AIDS strategy identifies youth aged 13-24 years as a priority population, based on increased risk for HIV transmission.8 While the seropositivity results presented in this report do partially represent this priority population, as almost 45% of all new HIV infections were identified in service members under 25 years of age, these results should not be generalized to the U.S. population. Data from HIV screening in U.S. military populations are based on a negative test prior to entry, as well as voluntary service. In countries with universal conscription, compulsory testing in samples of military recruits will be more representative of the young adult population.9 Following pre-accession screening of military recruits, routine screening represents relatively recently acquired HIV infections (i.e., infections acquired since the most recent negative test of each affected individual).
Routine screening of all civilian applicants for service and routine periodic testing of all active and reserve component members of the services have been fundamental components of the military’s HIV control and clinical management efforts.10 Previous MSMR reports presented HIV screening results for civilian applicants to the military service; however, these data are no longer available in the Defense Medical Surveillance System (DMSS), as the U.S. Military Entrance Processing Command stopped reporting data to the DMSS at the end of calendar year 2020. Thus, the data presented in this report reflect service members who had a negative HIV test upon entry to military service, followed by a positive test during uniformed service.
The mid-year 2023 HIV seropositive results for Navy and Marine Corps service members were obtained by the Navy Bloodborne Infection Management Center from the Navy’s HIV Management System. Due to changes in data processing, positive specimens are no longer accessioned in DoDSR, although non-positive HIV samples remain documented in DoDSR and accessioned through DMSS. Consequently, the total number of positive HIV tests were acquired from DMSS to calculate seropositivity rates. The total number of HIV tests completed as of June 2023 for Navy and Marine Corps active component service members approximated half of the tests completed during 2022.
The substantial declines in detection rates associated with routine screening for Army and Air Force service members should be more fully investigated at the end of 2023. If post-accession detection rates continue to decline through routine screening of the full military force, a cost-effectiveness analysis of universal versus indications-based testing after military enlistment may be warranted. Additionally, future studies should fully describe seropositivity rates by age and race, to further elucidate trends for the most at-risk populations. Health-seeking behaviors and co-morbidities should also be evaluated to identify those at highest risk for HIV infection.
References
- Department of Defense Instruction 6485.01, Human Immunodeficiency Virus (HIV) in Service Members (Change 2) 2013. Accessed August 11, 2023. https://www.esd.whs.mil/portals/54/documents/dd/issuances/dodi/648501p.pdf
- Secretary of Defense Memorandum for Senior Pentagon Leadership, Commanders of the Combatant Commands, Defense Agency and DOD Field Activity Directors. Policy Regarding Human Immunodeficiency Virus-Positive Personnel Within the Armed Forces. June 6, 2022. Accessed August 11, 2023. https://media.defense.gov/2022/Jun/07/2003013398/-1/-1/1/policy-regarding-human-immunodeficiency-virus-positive-personnel-within-the-armed-forces.pdf
- Brown AE, Brundage JF, Tomlinson JP, Burke DS. The U.S. Army HIV testing program: the first decade. Mil Med. 1996;161(2):117-122.
- Office of the Assistant Secretary of Defense. Health Affairs Policy Memorandum—Human Immunodeficiency Virus Interval Testing. HA Policy 04-007. March 29, 2004.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense Instruction 6485.01. Human Immunodeficiency Virus (HIV) in Military Service Members. June 7, 2013.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense Instruction 6130.03, Medical Standards for Appointment, Enlistment, or Induction in the Military Services. May 6, 2018.
- Army Medical Surveillance Activity. Supplement: HIV-1 in the Army. MSMR. 1995;1(3):12-15.
- White House Office of National AIDS Policy. National HIV/AIDS Strategy (2022-2025). Accessed September 6, 2023. https://www.hiv.gov/federal-response/national-hiv-aids-strategy/national-hiv-aids-strategy-2022-2025
- United States Department of Health and Human Services, Centers for Disease Control and Prevention. Introduction to HIV Sero-surveillance. Accessed September 6, 2023. https://globalhealthsciences.ucsf.edu/sites/globalhealthsciences.ucsf.edu/files/sero-surveillance_22sept09.pdf
- Okulicz JF, Beckett CG, Blaylock JM, et al. Review of the U.S. military’s human immunodeficiency virus program: a legacy of progress and a future of promise. MSMR. 2017;24(9):2-7.